The world of veterinary medicine continues to evolve and with it comes new treatment modalities.
Platelet rich plasma (PRP) is a prime example of this evolution. For years it has been used in human medicine to help with bone grafts, heal tendon and ligament lesions and promote wound healing. It was not until recently that PRP therapy and its benefits has made its way over to veterinary medicine.
To find out more, please watch the video below.
What exactly is PRP and why is it beneficial?

Platelet Rich Plasma is an autologous (self-derived) conditioned plasma that contains a high concentration of platelets. Platelets contain numerous growth factors that facilitate tissue repair and healing. These growth factors are contained in the alpha granule portion of the cell and are released from the platelet when it is activated (usually at an area of injury). A few examples of these growth factors are: Transforming Growth Factor β (TGF-β), Platelet Derived Growth Factor (PDGF), Insulin-like Growth Factor (IGF-1), Vascular Endothelial Growth Factor (VEGF), Epidermal Growth Factor (EGF) and Fibroblast Growth Factor (FGF). Roles of these growth factors range from vessel development and repair, to cellular recruitment and activation.
Many of these growth factors have been shown in recent studies to promote cartilage health and reverse the cartilage breakdown seen with osteoarthritis. Platelets have been shown to recruit and activate stem cells and PRP is increasingly being used in combination with stem cell therapy to augment the effects.
What can PRP be used for?
In veterinary medicine, PRP has been used for a wide range of indications including acute and chronic soft tissue injuries, osteoarthritis and even certain spinal conditions. Because PRP is obtained from the patient’s own blood, there is minimal risk and the positive effects of treatment can last for up to 6 months. In addition to these benefits, PRP is relatively inexpensive and can be done at patient-side in less than 30 minutes.
We use the Companion CRT system to produce high quality validated PRP in house without the need to send samples to external laboratories for processing.
The Companion Regenerative Therapies PurePRP® kit is the best performing platelet concentrating system in the veterinary market. This system is specifically validated for use in canine patients, and provides the optimal concentration of platelets while effectively removing more than 95% of Red Blood Cells and 85% of Neutrophils. (Carr, B, Canapp, S. et al. “Canine Platelet Rich Plasma Systems: A Multicenter, Prospective Analysis.” (2015) Front Vet Sci. 2015; 2: 73). Greenside Veterinary Practice was the first practice in the UK to use this system as all other PRP systems available in the UK were either not validated for canine patients or produced a product that failed to meet all the criteria for medical PRP properties.
The Companion Regenerative Therapies (CRT) system has been specifically validated for use in canine patients. In a multicenter study*, the CRT Pure PRP system was the only system that increased platelet concentration while significantly reducing the red blood cell and neutrophil concentrations.
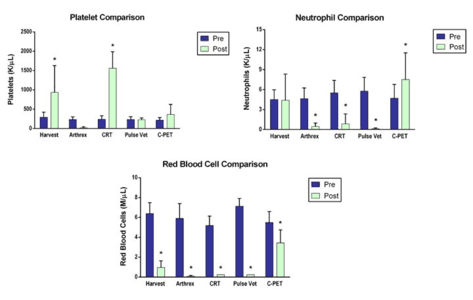
Why is it Important to Reduce Neutrophils and Red Blood Cells (RBCs)?
The goal is to obtain the highest concentration of platelets and growth factors, whilst removing the other blood components such as the red and white blood cells, which can cause pain and inflammation.
White blood cells: Neutrophils:
- Multiple studies show that neutrophils increase concentrations of unwanted inflammatory mediators (IL-1β, TNF-α, IL-6, IL-8)
- Increased concentrations of neutrophils in PRP is positively correlated with an increased MMP-9 concentration, which leads to degradation of collagen and other extracellular matrix molecules. Neutrophils should therefore be removed from PRP products.
Red Blood Cells:
- RBC’s damage cartilage and synovium directly via iron-catalyzed formation of Reactive Oxygen Species (ROS)
- RBC’s increase concentration of unwanted inflammatory mediators (IL-1 and TGF-α)
- PRP with high concentration of RBC’s caused significantly more synoviocyte death when compared to PRP preparations with lower RBC count.
References:
Braun HJ, et al., Am J Sports Med. 2014
Sundman EA, et al. Am J Sports Med. 2013
* Carr, B, Canapp, S. et al. “Canine Platelet Rich Plasma Systems: A Multicenter, Prospective Analysis.” (2015) Front Vet Sci. 2015; 2: 73
What should I expect if my pet has a PRP injection?
PRP is commonly given as a single injection but sometimes repeat injections are required two weeks apart. For certain conditions or advanced osteoarthritis PRP is combined with stem cells and injected into the joint. Approximately 50% of dogs require more than one injection for a significant improvement, however this is dramatically reduced if it is combined with stem cell therapy. PRP therapy is a minimally invasive procedure that is performed in house under sedation.
Approximately 30 to 60 ml of blood is collected from the jugular vein which is then processed and prepared for injection. The patient is sedated and the treatment site clipped and aseptically prepared. For joint injections a needle is placed into the joint and arthritic joint fluid removed and replaced with PRP. For soft tissue injuries, ultrasound guidance is used to ensure accuracy of administration directly into the lesion. PRP can also be used to speed the healing of wounds and burns and we commonly use it combined with Manuka honey in wound dressings.
In people, mild discomfort has been reported following the injection for the first 24-72 hours and this can be managed with cold compresses and pain medication prescribed by us if required. Following treatment your pet will be rested for two weeks and then an appropriate rehabilitation program started to help with the regenerative process.