Elbow dysplasia (ED) is one of the most common causes of thoracic limb lameness in Labradors and other large and giant breed dogs and it is seen very frequently in our clinic.
Elbow dysplasia (ED) is one of the most common causes of thoracic limb lameness in Labradors and other large and giant breed dogs and it is seen very frequently in our clinic. ED is a term used to describe the presence of one or more developmental conditions involving the elbow joint. These conditions develop in juvenile animals and pain and lameness are often present at four to six months of age. Many dogs do not present until much later when osteoarthritis (OA) is advanced and lameness is a constant feature.
There have been many techniques described for both medical and surgical management of ED. Surgical options include arthroscopic interventions, ulnar osteotomies, proximal ulnar osteotomy, distal ulnar osteotomy, biceps ulnar release procedure, proximal abducting ulnar osteotomy, sliding humeral osteotomy, canine unicompartment elbow replacement, full elbow replacement and elbow arthrodesis. However, irrespective of which medical or surgical intervention is performed, ED will lead to cartilage damage and degenerative osteoarthritis (OA) with time. The only exception to this would be for full elbow replacement but this procedure is not currently recommended due to the high complication rate.
The sheer number of treatments proposed for this condition tells us that not one is highly effective and also that the elbow joint is incredibly complex and is not easily replicated with implants for joint replacement. Surgical and arthroscopic interventions are done to try to control pain and limit osteoarthritis development that inevitably ensues with time. However, in many cases this is not successful.
Should we be looking at this disorder in a different way? At Greenside we think it should. Accordingly, we have pioneered a novel treatment strategy that takes a different approach. This minimally invasive treatment targets the joint using the body’s own repair kit to prevent or reverse the degenerative changes that occur.
At Greenside, we are seeing an epidemic of ED cases; primarily, they are cases in which the animals have undergone various treatments but remain lame due to chronic pain from secondary osteoarthritis. We also see many cases where ED has been recently diagnosed and the owners are seeking alternative treatment options to surgery or conservative management. The story of Magic and Merlin’s treatment for ED at Greenside demonstrates the effects of arthroscopic interventions and regenerative medicine (RM).
Magic and Merlin are two brothers from the same litter. Magic was presented at his first opinion vet at nine months old due to intermittent thoracic limb lameness. A course of NSAIDs improved the lameness but did not resolve it. Magic underwent CT imaging and was diagnosed with bilateral ED with a fragmented medial coronoid process (FCP). The left elbow was treated with arthroscopy by removing the FCP and curetting out the damaged cartilage. A similar procedure was recommended for the right elbow at a later date after recovering from the procedure to the left elbow. Magic responded poorly to the arthroscopic intervention and the lameness persisted and worsened with time. The owners were not keen on performing the same surgery on the right elbow and looked for other options. Six months following the arthroscopy Magic presented at Greenside Regenerative Therapies clinic to start treatment in both elbows with regenerative medicine. At this time, bilateral hip dysplasia was also diagnosed, and repeat radiographs of the left elbow revealed extensive OA had already formed in the joint.
Magic underwent a small fat harvest procedure from the falciform ligament under general anaesthesia. The fat was shipped to an external laboratory where it was processed to extract the adipose derived mesenchymal stem cells. These were culture expanded and then returned to Greenside cryogenically frozen. Four weeks after the fat harvest Magic was sedated and his elbows and hips were clipped and aseptically prepared. Blood was taken and spun in a special concentrating device in a centrifuge to separate and concentrate his platelets to form leukocyte poor platelet rich plasma (PRP). His stem cells were defrosted and combined with an equal volume of PRP and injected into both elbows and hips.
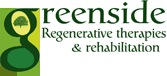
Magic’s lameness improved over the following eight weeks and by 12 weeks following implantation he was no longer lame and was not receiving any analgesic medications. The range of motion in both elbows had improved significantly although the flexion angles (as measured by goniometry) were larger on the left, indicating that some restriction was still present. Stance analysis revealed a normal weight distribution in all four limbs. Magic did very well for 18 months following treatment but he then presented with a mild left thoracic limb lameness again. Repeat radiographs revealed Grade 4/5 OA in the left elbow and Grade 1.5/5 OA in the right (Figure 1).
Magic.
A second treatment of autologous stem cells and PRP was given and Magic’s lameness resolved again without the requirement for pharmacological intervention. It was interesting to see that the OA in the left elbow was more advanced than on the right, despite both elbows having the same initial diagnosis of ED and FCP. The only difference was that the left elbow had had the FCP removed and the cartilage curetted. For this case, arthroscopic intervention did not resolve the pain and lameness and also did not prevent the formation of severe OA. Two recent publications have shown that there is no significant difference in the long-term outcomes for dogs with ED treated with arthroscopic intervention when compared to conservative management. This does require further study as with such a common procedure such as elbow arthroscopy, it raises the question of whether this should continue to be performed for these cases.
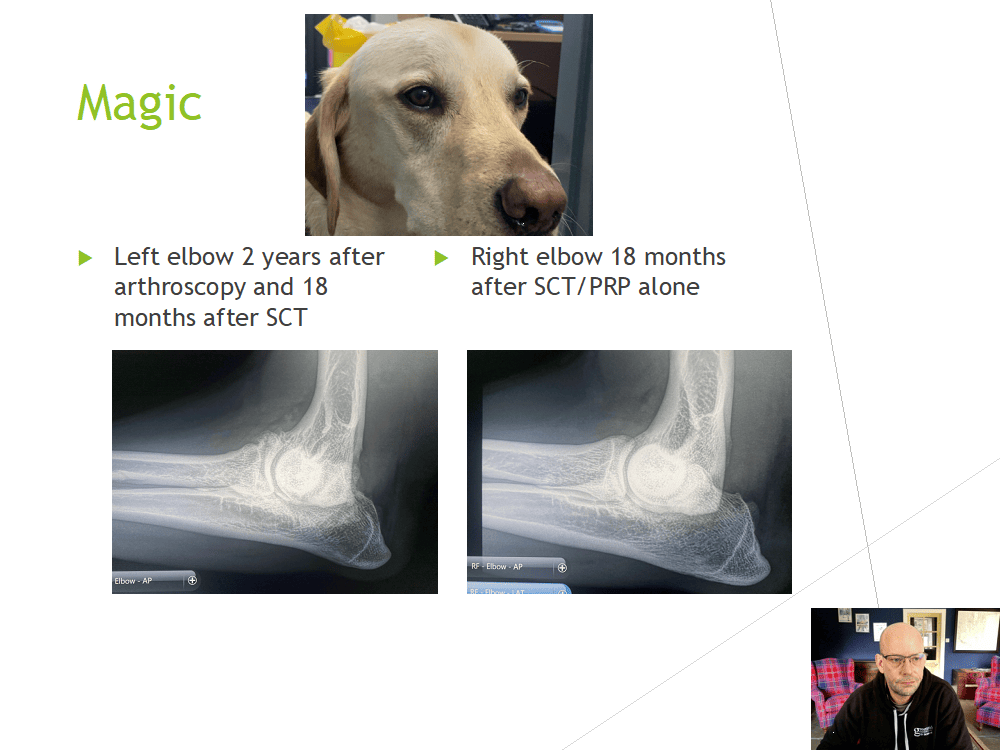
Figure 1. Lateral radiographs of Magic’s elbows, two years after arthroscopic intervention
in the left and 18 months following stem cell therapy and PRP in both.
Merlin is Magic’s brother from the same litter, and he became lame at twelve months old. Considering the history of his brother who had presented at a younger age for lameness, Merlin underwent the same diagnostic investigations in both elbows and hips. Radiographs revealed bilateral hip dysplasia and suspected elbow dysplasia. CT Scans confirmed the diagnosis of ED with FCP. Due to the owners’ experience with his brother, Merlin did not undergo arthroscopy and was presented immediately to start treatment with regenerative medicine. He had fat harvested and autologous stem cells were cultured. He underwent stem cell therapy in combination with PRP into both elbows and hips and his lameness resolved and he was managed without the need of analgesics for two years. When Merlin presented for mild lameness again two years later, repeat radiographs of both elbows revealed no deterioration in the sub trochlear sclerosis and the OA had not progressed (Figure 2.)
Merlin.
When we compare these two cases with identical diagnoses, identical environmental factors and similar genetics due to being siblings, we can see that RM is a highly effective treatment option to prevent the degenerative changes in the elbow joint following developmental abnormalities resulting in ED. What is also highlighted in these cases is that Magic’s arthroscopic intervention (AI) did not prevent or delay severe OA from forming and that treatment with RM in a joint that has undergone AI is more challenging with reduced treatment response times. These cases highlight something that we have seen hundreds of times in our patients: that RM can effectively turn off the degenerative process within the joint, providing a sustained long-lasting treatment for OA.
Figure 2. Lateral radiographs of Merlin’s elbows at diagnosis and two
years following treatment with regenerative medicine.
At Greenside, we have been using stem cell therapy along with PRP to treat ED for a number of years and have modified our protocols with experience to develop a minimally invasive, highly effective treatment option. Using RM, we are able to stop the degenerative process, reverse some of the signs of OA and restore joint health. Although RM cannot reverse the process (the dysplasia or abnormal development of the elbow joint) that results in the formation of OA, we have shown it to be highly effective in managing the condition with outcomes and longevity of effects that outperform many surgical interventions and conservative management. We are able to resolve lameness, reduce pain and improve function for extended periods of time. Positive treatment responses commonly last for 18 months to two years before a top up injection is required. Because RM cannot reverse the underlying ED, with time, the joint will start to degenerate again. At this point further treatment can be provided to regain control and arrest the degenerative process.
Once stem cells have been harvested from the patient, we can also cryopreserve them, which means we have a supply of stem cells - typically for the lifetime of the patient. When a further treatment is required, we can simply wake these cells up at the lab and culture more without having to harvest more adipose tissue from the patient. Culturing the stem cells has many advantages, such as knowing the exact concentration and viability of cells to provide a reliable “dose” specific to the condition being treated. The sterility, morphology and purity of the resultant cultured stem cells are checked prior to shipment from the lab to ensure patient safety and ensure the best possible cells are used.
From our extensive experience of treating ED, we have found that dogs that have undergone arthroscopic intervention prior to treatment with RM tend to do less well than those dogs not having the procedure. We believe this is due to the invasive nature of arthroscopy and for the potential to cause further instability and more severe OA changes following FCP removal and curetting of the cartilage. For this reason, we do not advocate the use of arthroscopy to manage ED.
Not all stem cell treatments and PRP therapies are the same and many have not been validated in dogs, which can result in sub optimal treatment outcomes.
At Greenside we have investigated and trialled many different products and we believe we have found and validated the best possible products to ensure successful and consistent positive treatment outcomes.
Greenside Regenerative Therapies and Rehabilitation was the first specialist referral centre in the UK to provide treatments using stem cell therapy and rehabilitation and we use objective data to ensure our patients are improving and to modify treatments using an evidence-based approach rather than subjective-only assessment. After treatment, we monitor our patients and provide support, including home exercise plans and rehabilitative therapies. We offer regular reassessments and remote support as required. There is no cure for ED, but Greenside has developed a more efficacious treatment option, resulting in reduced pain, increased function and a better quality of life for hundreds of dogs.